What exactly is brain fog? Here’s what scientists are finding out.
Scientists have long struggled to define brain fog—let alone pinpoint a cause for it. But research is starting to reveal multiple potential causes from inflammation to a leaky blood-brain barrier.
After a COVID-19 infection, many patients found themselves in a fog. Their attention wandered, their memory faltered. They felt sluggish, had trouble thinking straight, and struggled with basic chores.
These patients were experiencing brain fog, a symptom that plagues 20 to 65 percent of people with long COVID—a wide range of estimates that underscores how little understood it is. But while brain fog’s association with COVID has popularized the term, it was actually first used in chronic illness communities.
Patients report brain fog as a consequence of chronic conditions including fibromyalgia, myalgic encephalomyelitis/chronic fatigue syndrome, and lupus. Many people also report brain fog after chemotherapy or taking drugs, like pain relievers. And it’s associated with mental health issues, like depression and schizophrenia.
(Is long COVID forever? A new study has clues.)
Across these different conditions, patients point to similar symptoms: difficulty concentrating, forgetfulness, confusion, and cognitive slowness or cloudiness, says Jacqueline Becker, a neuropsychologist at Icahn School of Medicine Mount Sinai. Often, it’s among the most debilitating symptoms patients with chronic illness experience. “It can really take over people’s lives,” Becker says.
For many patients, the cause of their brain fog has been hard to pin down. Recently, however, scientists have made some breakthroughs in understanding what might provoke it in some conditions—particularly long COVID—and how to treat it.
What brain fog is—and what it isn’t
While there is no universally agreed upon definition of brain fog—and many experts debate how useful the term is in a clinical setting—most scientists consider it to be a set of symptoms of an underlying condition rather than a diagnosis. “Brain fog has become a catch all for all of the broader neurological symptoms of certain conditions like long COVID,” Becker says.
As to why so many different conditions cause similar symptoms, it might be because brain fog can point to deficits in many areas of cognition, including attention, concentration, or ability to execute tasks, says Avindra Nath, intramural clinical director of the National Institute of Neurological Disorders and Stroke. “If the brain isn’t functioning properly, people call it brain fog.”
Yet experts distinguish brain fog from cognitive impairment, the latter of which results in deficits in memory or attention that can be measured. Patients with brain fog often report problems with attention and memory, but clinicians can’t always find measurable deficits in these areas. Sometimes, patients with brain fog undergo a battery of tests, only for everything to come back normal, she says. “That can be really frustrating for patients,” Becker says.
Physicians sometimes dismiss the brain fog as purely psychological in nature. This is particularly true for people with chronic conditions or long COVID, who often feel like their providers aren’t taking them seriously, Becker says.“There is a prevailing perspective that long COVID,” has a purely psychiatric origin, she says. “And I think it's important to challenge that.”
Even though brain fog may look the same across the many conditions linked to it, scientists are starting to agree that it likely has many different potential causes, says Peter Denno, a clinical fellow at Imperial College London, who wrote a recent review of the subject. And those causes influence how—and whether—it can be treated.
A link between inflammation and brain fog
Recently, scientists have started to understand the link between inflammation and brain fog, opening up avenues for diagnosis and treatment.
“One of the biggest hypotheses for what underlies brain fog in all of these different conditions is neuroinflammation,” Becker says.
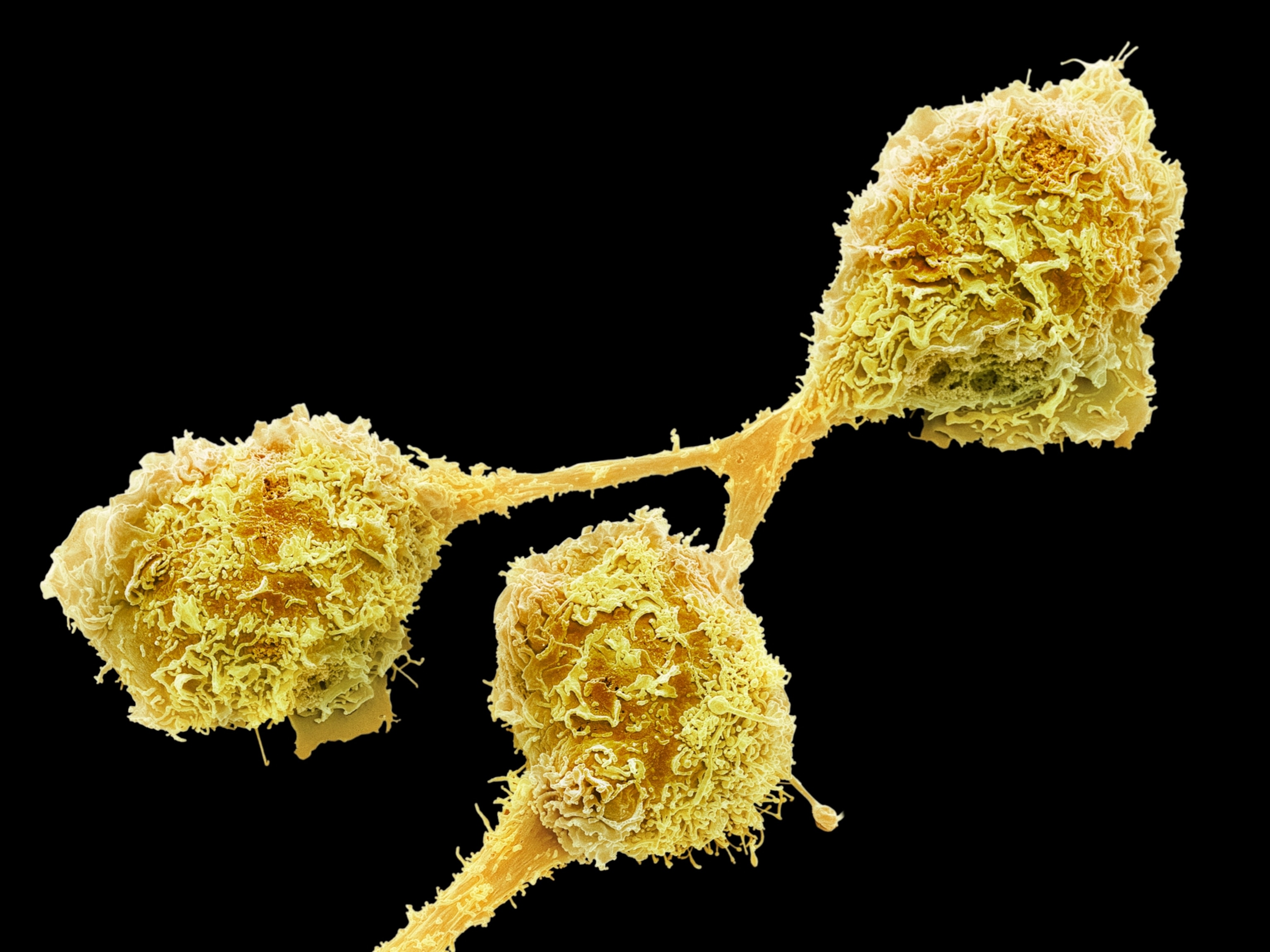
Mounting evidence shows that COVID-19 triggers an overactive or misdirected immune response that may continue to afflict patients even once they have recovered from the disease’s most acute symptoms.
(The end of inflammation? New approach could treat dozens of diseases.)
For example, studies show that a COVID infection can cause the long-term activation of the brain’s immune cells and impair neuronal growth in patients with brain fog. Some patients also start to produce autoantibodies, which signal the immune system to attack healthy tissue, including cells in the brain. Studies further suggest that COVID-induced inflammation can cause long-term reductions in brain’s gray and white matter size, leading to cognitive deficits.
Scientists hypothesize that these lingering viral reservoirs in the brain might cause persistent inflammation in the brain among long COVID patients as their immune systems continue to fight off the virus. Studies have found similar patterns of inflammation in chronic fatigue syndrome, post orthostatic tachycardia syndrome, and chemo fog.
Brain fog and the leaky blood-brain barrier
More insight into brain fog came in a study published in Nature in February 2024. In the study, Colin Doherty, a neurologist at Trinity College Dublin Medical School, and his team scanned the brains of long COVID patients. In addition to systemic inflammation, they found that patients with brain fog had leaky blood-brain barriers, the highly selective membrane that protects the brain from toxins, viruses, and other harmful molecules.
They hypothesize that a leaky blood brain barrier could allow these substances into the brain, causing neuroinflammation and disrupting the brain’s normal metabolic processes.
Other studies have found similar blood-brain barrier dysfunction in patients with autoimmune disorders, including lupus and chronic fatigue syndrome.
Other experts caution that this study was small, so it's hard to draw too many conclusions. Denno also points out that another study published in March 2024 failed to show a correlation between brain fog and blood brain barrier disruption. That could be because Doherty’s study included people who had objective cognitive performance deficits, Denno says.
Other potential causes of brain fog
Scientists are investigating other possible causes of brain fog too. Studies show that changing hormone levels can also cause profound changes in the brain. In patients undergoing menopause, for example, declining estrogen levels are thought to cause reductions in the size of some brain areas, perhaps contributing to cognitive haziness.
Meanwhile, in patients with hypothyroidism, thyroid hormone deficiency is also thought to decrease the volume of certain brain areas, mainly the hippocampus. And in patients with traumatic brain injury, their brain fog-like symptoms have been linked to low levels of growth hormone.
Some scientists also speculate that dysfunction of the gut microbiome might lead to brain fog in some cases, as one small study published in October 2024 found evidence of brain fog in more than half of participants with gastrointestinal diseases like inflammatory bowel syndrome. Scientists hypothesize that changes to the gut microbiome might play a role in long COVID-related brain fog too, and some research suggests that a microbial imbalance in the gut might contribute to neuroinflammation.
But in many other conditions, scientists haven’t found out much about the biology of brain fog. That’s because there have been very few high-quality studies on brain fog in general, Denno says. And the higher quality studies that have specifically looked into brain fog are often inconsistent in their results and methodology. The link between brain fog and chronic pain, for example, remains murky for this reason, researchers argue.
Denno argues the medical field might be better off considering the cognitive symptoms that come with each disease separately and adopt a more consistent methodology to study brain fog.
Clearing up (and diagnosing) brain fog
While there may not be one single cause of brain fog, there are some things people can do to combat it, experts say. If you’re experiencing brain fog, Becker suggests first looking at lifestyle factors, such as exercise, healthy eating, and getting enough sleep. But people that experience intense brain fog or fog that lastsmore than a few weeks should consult a physician, she adds.
Clinicians can assess whether there’s a reversible cause of brain fog, like sleep apnea, vitamin B deficiency, and other hormone and thyroid issues. They can also look for signs of inflammation and neurodegenerative markers, says Nath.
People with more significant, measurable cognitive impairment can benefit from cognitive rehabilitation therapy, Becker says. “It’s a benign treatment with a lot of really great benefits.” Nath likens cognitive rehabilitation therapy to exercise for the brain. “What we do is they exercise the brain in the domains where there’s a deficit,” he says.
There might be new drug treatments on the horizon. Some patients, particularly those with chemo-related brain fog, have found relief taking medications used to treat ADHD, Becker says. Some smallstudies have found that antihistamines or famotidine, an antacid with anti-inflammatory properties, can help decrease inflammation and relieve brain fog.
Nath and his team are also studying the effects of intravenous immunoglobulin, an antibody that is used to treat immunological disorders like lupus, on long COVID. The theory is that it will suppress the immune system’s excessive inflammatory response, which would in turn keep the body from damaging healthy cells and alleviate brain fog. Next, they also want to try using checkpoint inhibitors, a type of immunotherapy typically used to help the body's immune system fight cancer, in cases of long COVID, too.
But experts agree that researchers need to learn more about brain fog first before they can get a better handle on it. “There’s this idea in medicine that if we can’t break a symptom down into a latinized medical term then we’ve failed,” Doherty says. Instead, it just might be a reason to keep investigating.