Everybody is tempted to pop zits—but is there a safe way?
Can popping zits in this area cause infection and even death? Dermatologists weigh in on the viral claims, and how to take care of your skin.
You may have seen claims that popping pimples in the triangle from the bridge of the nose to the corners of the mouth could cause serious infection, and even death.
There is real cause for concern about infections in this area, called “the danger triangle” or “triangle of death,” but experts say serious infection here is incredibly rare. That said, they agree the recent increased caution around pimple popping is a good thing.
Why exactly is the danger triangle treated with increased care, and what are the risks of popping zits in general? Though dermatologists universally recommend leaving blemishes untouched, they acknowledge it’s unrealistic to expect everyone to heed their advice. They break down the science of how to deal with aggravating acne at home, and when to get help from a dermatologist.


What is the triangle of death?
Popping pimples in the “danger triangle” most likely won’t kill you, says Joshua Zeichner, associate professor of dermatology at Mount Sinai Hospital. In a few rare cases, however, infections in this area have led to serious complications including partial facial paralysis.
That’s because the central part of the face is rich with blood vessels which drain into a structure known as the cavernous sinus, a hollow region behind the eye sockets that has a direct connection to the brain, Zeichner says. Bacterial infections in this area can trigger blood clots that can travel to the brain, a life-threatening condition known as cavernous sinus thrombosis.
However, “it’s very unlikely that picking a pimple will truly lead to an infection that will spread to the sinus,” let alone reach your brain, he says. Even though popping a pimple creates a small open wound, it typically doesn’t introduce enough bacteria to cause an infection that is deep enough to reach the sinus. Just like small cuts elsewhere on the body, immune cells in the skin are effective at stopping an infection inside the pore before it reaches the blood.
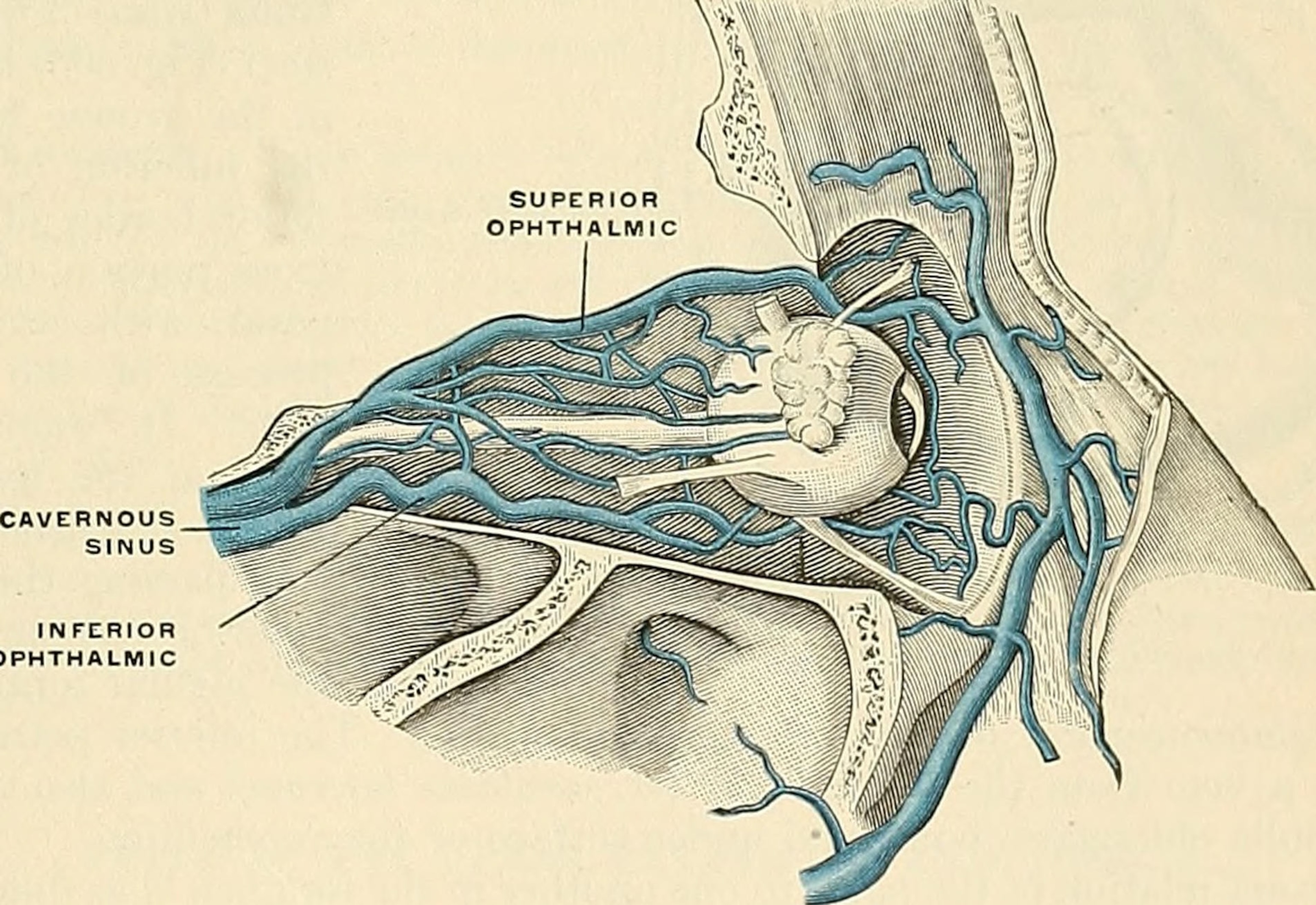
Jordan Carqueville, the founder and medical director of the Derm Institute of Chicago, says that careful surgical technique is necessary when performing invasive procedures in the “danger triangle.” Because of the dense network of blood vessels in this area, it is prone to excessive bleeding, which can result in blood clotting and collection outside of the blood vessels, and potentially cause tissue damage or infection.
But she adds that in her twenty years as a dermatologist, she hasn’t encountered a cavernous sinus infection—let alone one caused by a pimple. “This situation of death being caused by popping a pimple in this area is exquisitely rare,” she agrees.
That doesn’t mean that you should pop pimples, however, especially in the danger triangle. While the term might be dramatic, the concept “does shed light on the importance of proper skincare and avoidance of bad habits that can lead to an infection,” Zeichner says.
Popping a pimple anywhere might lead to infection, discoloration, or permanent scarring, Zeichner says. The risk of spreading an infection might be higher in these blood vessel-rich areas of the face.
In general, don’t pop your pimples
Even outside the triangle of death, experts agree “it’s always safer not to pop” zits, says Sandra Lee, a dermatologist and YouTuber popularly known as Dr. Pimple Popper. “There’s very few instances when a pimple needs to be popped,” adds Jayden Galamgam, a dermatologist at UCLA.
Pimples occur when pores or hair follicles become clogged with skin oils or dead cells, causing bumps called comedones. The two most common types of pimples are closed comedones and open comedones. With open comedones, also known as black heads, the substance inside oxidizes, causing the pore to appear black. It’s common practice for estheticians and dermatologists to extract black heads from the skin—and that’s safe, experts say.
Closed comedones, on the other hand, occur when pores become totally clogged and the skin closes up around it. These pimples appear as small bumps that may or may not have a white head. Closed comedones can also trigger an immune response, causing red, pus-filled, and sore bumps deeper within the skin, known as inflammatory acne. If you pop any of these types of pimples, odds are you’re going to do more harm than good, especially for painful red bumps without a white center.
The act of popping closed comedones can set off an inflammatory cascade that can make the area look redder. You’re also potentially spreading the bacteria in the pimple, which can lead to a deeper infection, changes in skin pigmentation, and scarring, Galamgam says.
To manage pimples without popping, Carqueville recommends hydrocolloid bandages, also known as pimple patches. These not only help pimples clear more quickly by keeping the area moist, preventing picking, and protecting the area from bacteria, but also put pimples out of sight and hopefully out of mind.
If a pimple isn’t clearing up, it’s best to go to a dermatologist to discuss your options. Zeichner says that sometimes, extractions might be the best way to clear up a clogged pore that isn’t going away on its own.
Popping pimples safely
Realistically, experts recognize that it’s difficult to leave pimples alone. If you just can’t help it, treat it like a surgical procedure, Zeichner says. That means cleaning and disinfecting the skin, hands, and any instruments with soap and water or alcohol to minimize the chance of bacteria making it into the pimple.
Lee says that it’s also important to make sure the pimple is ready to come out, meaning that it’s come to a head, and to stop trying to pop it if nothing is happening. If you’re using fingers, says Lee, wrap them in tissue, or, better yet, use a sterilized comedone extractor. Then, apply gentle, even pressure to the zit, Zeichner says, so you don’t leave a mark, which can take longer to heal than the pimple itself. After popping, Lee advises applying a bit of benzoyl peroxide with a clean cotton swab to disinfect the area.
But ultimately, “you cannot manage your acne by simply picking at it,” Lee says. In terms of over-the-counter medications, there are several products that can help people manage acne. “Salicylic acid is fantastic for unclogging pores and treating blackheads and whiteheads, while benzoyl peroxide is effective at killing acne-causing bacteria,” Lee says. Retinoids, which act like pipe cleaners for your pores, are also effective for managing acne, Zeichner says.
But there are also a lot of things that cause acne, some of which aren’t possible to control. Genetics, hormonal changes, and stress also play a role in acne formation. Everyone is different, he emphasizes.
If you have acne that isn’t clearing up, or you’re experiencing deep, painful, cystic acne, it's best to visit a dermatologist. Early treatment can prevent scarring and discoloration, which can be permanent.








