This is the worst flu season in 15 years. Here's why—and how to protect yourself.
The number of influenza cases is surging across the United States, putting significant strain on many hospitals. We asked the experts to explain what makes this year's flu season so unusual.
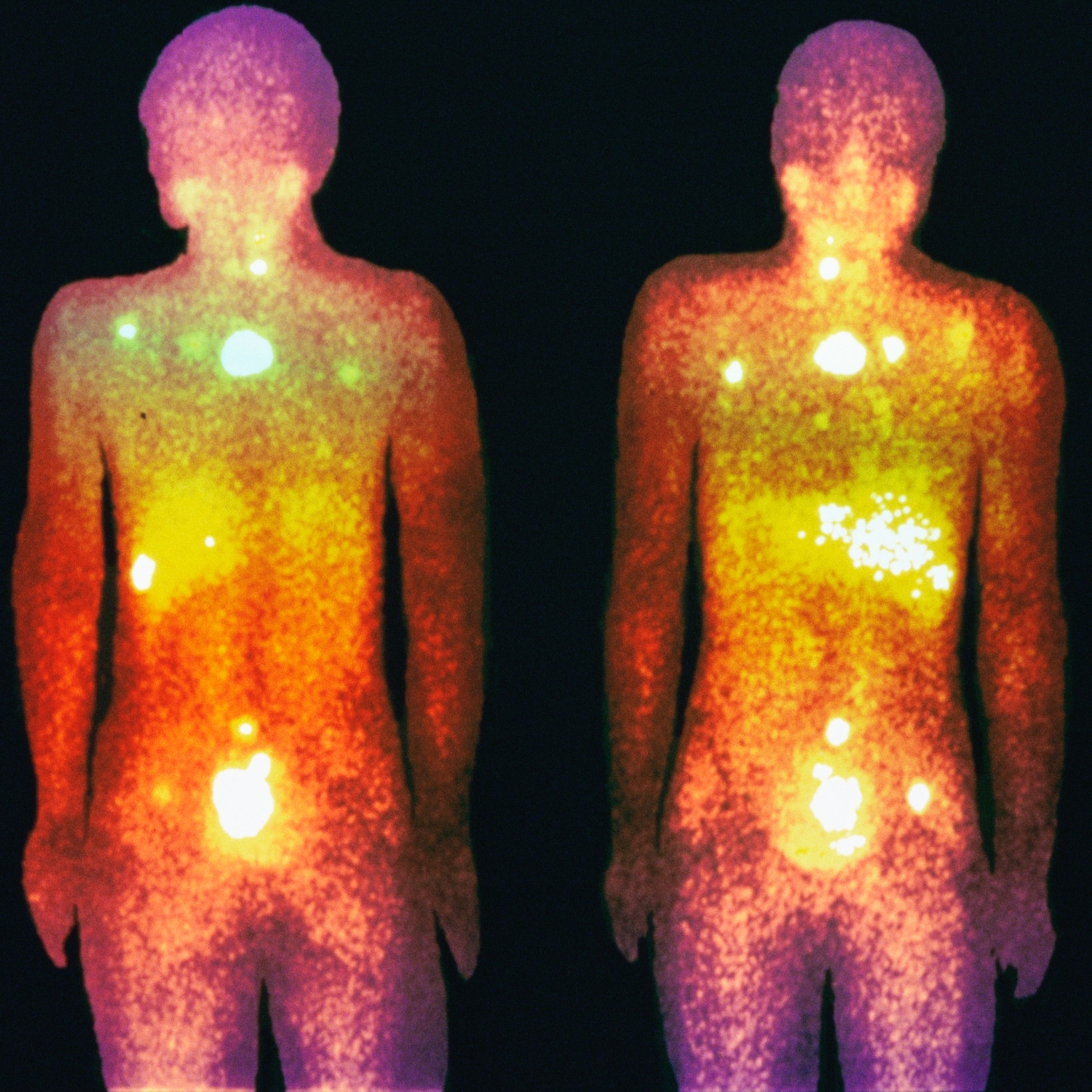
Seasonal flu cases have hit a 15-year high this year—filling hospitals, shutting down schools, and leading to an estimated 19,000 flu-related deaths so far in the United States. These deaths even topped winter COVID-19-related deaths for the first time since the pandemic began five years ago.
While flu cases surge, RSV, norovirus, and COVID-19 infections have also remained high, "putting a significant strain on hospitals—particularly as patients compete for the same resources such as intensive care unit beds and healthcare personnel," says Jason Nagata, a pediatrician at University of California, San Francisco Benioff Children’s Hospital. "Hospitals are struggling to keep up with the demand, and some have been forced to set up temporary triage tents."
Moreover, this flu season most closely resembles the 2019-2020 season, which saw peaks in December, February, and March. If a similar peak happens next month of this year, there could be even more devastation.
(Got a cold? Here’s how your immune system is fighting it.)
Here's what's contributing to this year’s remarkably high flu rates—plus what you can do to protect yourself and your family.
What's behind the 15-year high flu rates?
“It’s not always clear why flu seasons vary so much in severity," says William Schaffner, an infectious disease specialist at Vanderbilt University School of Medicine, but there are likely several factors contributing to this year’s significantly high numbers.
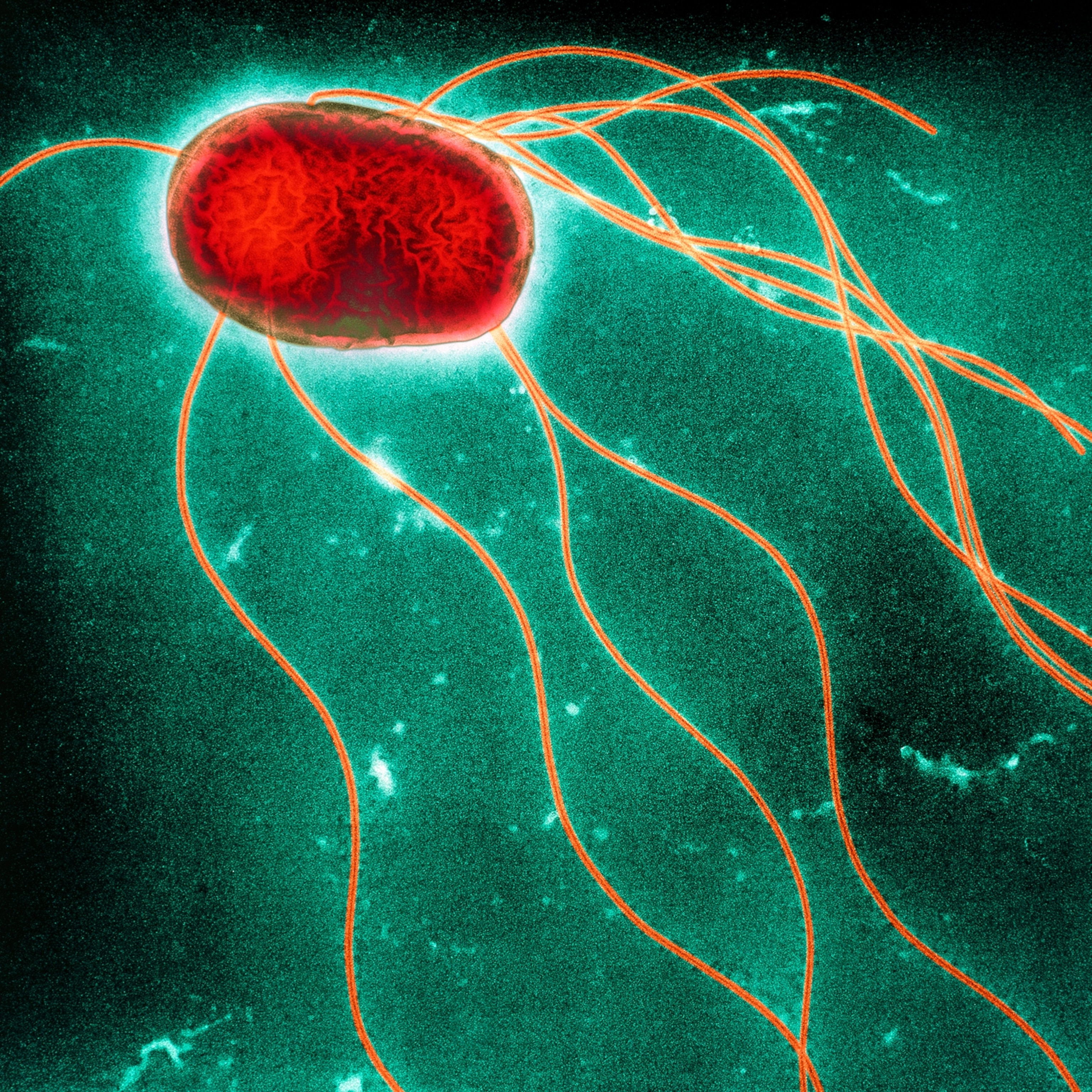
One component Schaffner points to is this year’s unusually cold winter "driving people indoors, thereby increasing close contact and making it easy for the virus to spread." Similar to RSV and COVID-19, influenza is transmitted through tiny respiratory droplets that are released when an infected person breathes, talks, coughs, or sneezes.
The U.S. is also likely still experiencing an "immunity gap" resulting from less exposure to the flu and other viruses during the pandemic due to COVID-19-related preventative measures, says Nagata. Precautions like social distancing and face mask use, while critical in preventing the spread of the coronavirus, led to fewer influenza cases during the pandemic and therefore fewer antibody development in individuals to protect against subsequent flu seasons like the one occurring now.

This flu season has also been "highly unpredictable," Nagata explains, with multiple waves of flu infections and both H1N1 and H3N2 strains circulating at the same time. The virus normally only sees one peak per season and has a strong predominance of one strain over another, so multiple peaks and two strains sharing the same stage is unusual.
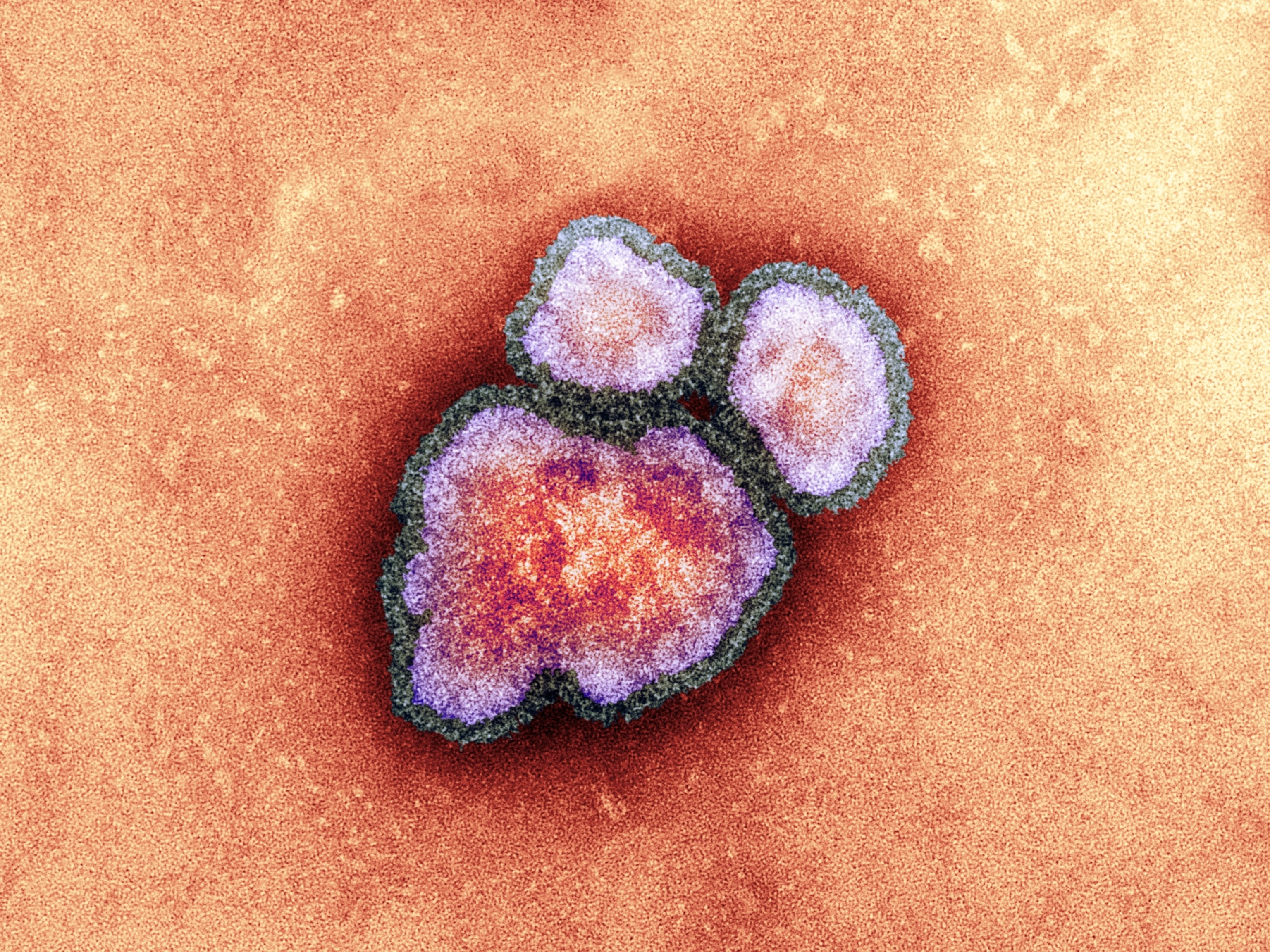
One preliminary report indicates that such unpredictability may have made this year's flu shots a poorer match with the virus than in previous years—but there isn't enough data yet to know if that's actually the case, explains Jason Newland, chief of infectious diseases at Nationwide Children’s Hospital in Ohio. "We do know that even in mismatched years or where the effectiveness isn’t as good, we still get some protection against severe disease," he says.
Likely the biggest contributing factor behind this year's abnormally high number of flu cases is that many people aren’t getting the vaccine at all. "Flu vaccination rates have declined, which is a major cause of the surge," says Elizabeth Mack, a physician and the head of the pediatric critical care unit at the Medical University of South Carolina’s Children’s Health.
(How the additives in your vaccines rev up your immune system.)
Data from the U.S. Centers for Disease Control and Prevention indicates that as of February 1, 146.5 million doses of the vaccine were given in the country, while data from the same week last year shows 156.9 million people received the shot—a 7 percent decline. “Flu vaccination rates are at their lowest level in years, with fewer than half of Americans currently immunized," says Nagata.
And despite children under five being especially vulnerable to the worst outcomes of influenza, less than 46 percent of kids have received a flu vaccine this year, "which is lower than last year at this time, [when] we saw more than 50 percent," says Leana Wen, an emergency physician and public health professor at the George Washington University Milken Institute School of Public Health.
How to protect yourself from the flu
Regardless of what's behind the current surge, "we know how to protect against influenza and how to treat it," says Newland.
(Chicken soup? Tea? Here’s what to feed your body when it’s sick.)
One of our most basic preventative tools is good hygiene. "Everyone should wash their hands well with soap and water—especially after touching commonly used surfaces," says Wen.
She adds that particularly vulnerable people such as very young children, pregnant women, the elderly, and the immunocompromised should consider additional precautions such as wearing a high-quality face mask in indoor public spaces and avoiding crowded, poorly ventilated areas.
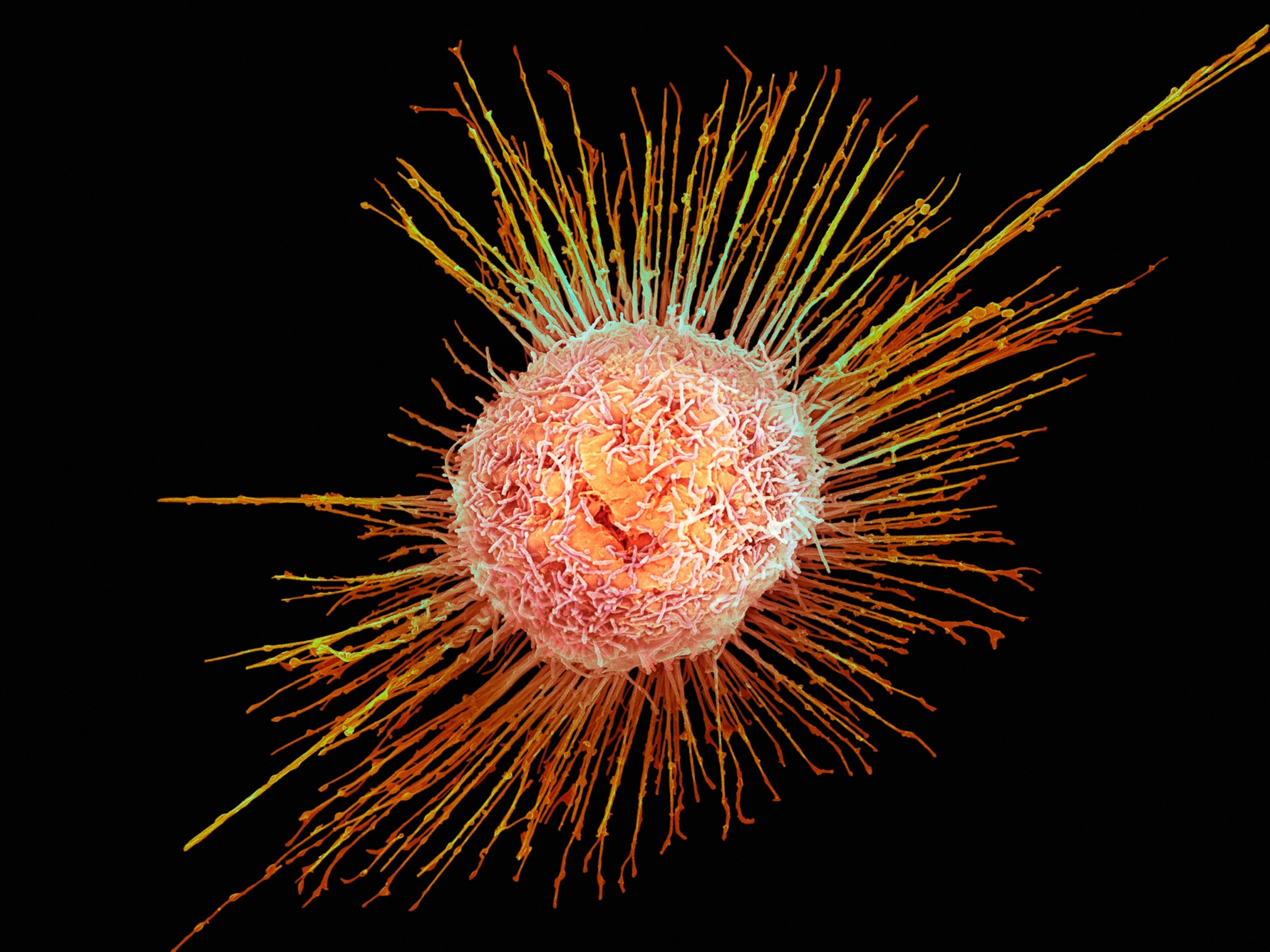
Maintaining a healthy lifestyle by getting enough sleep, eating nutritious foods, and staying active "can also strengthen your immune system and reduce your risk of infection," says Nagata.
But the most surefire protection against the worst outcomes of the virus likely comes from getting the flu shot. "That’s why it’s recommended that everyone six months of age and older get an annual influenza vaccine," says Mack. Although it takes about seven to 10 days for protective antibodies to develop in the body after receiving the shot, because this flu season could last at least another month, getting vaccinated is still encouraged.
It's important to remember that getting the vaccine won't entirely stop you from getting the flu, but it will reduce its severity if you do get infected, “and can keep you out of the hospital, ICU, and prevent you from dying," says Schaffner. "It turns wild into mild."