To fight malaria, scientists want to poison mosquitoes—with human blood
Low doses of a drug already approved for treating rare genetic conditions in humans kills mosquitoes dead. Scientists say it could be a valuable new tool in the fight against disease.
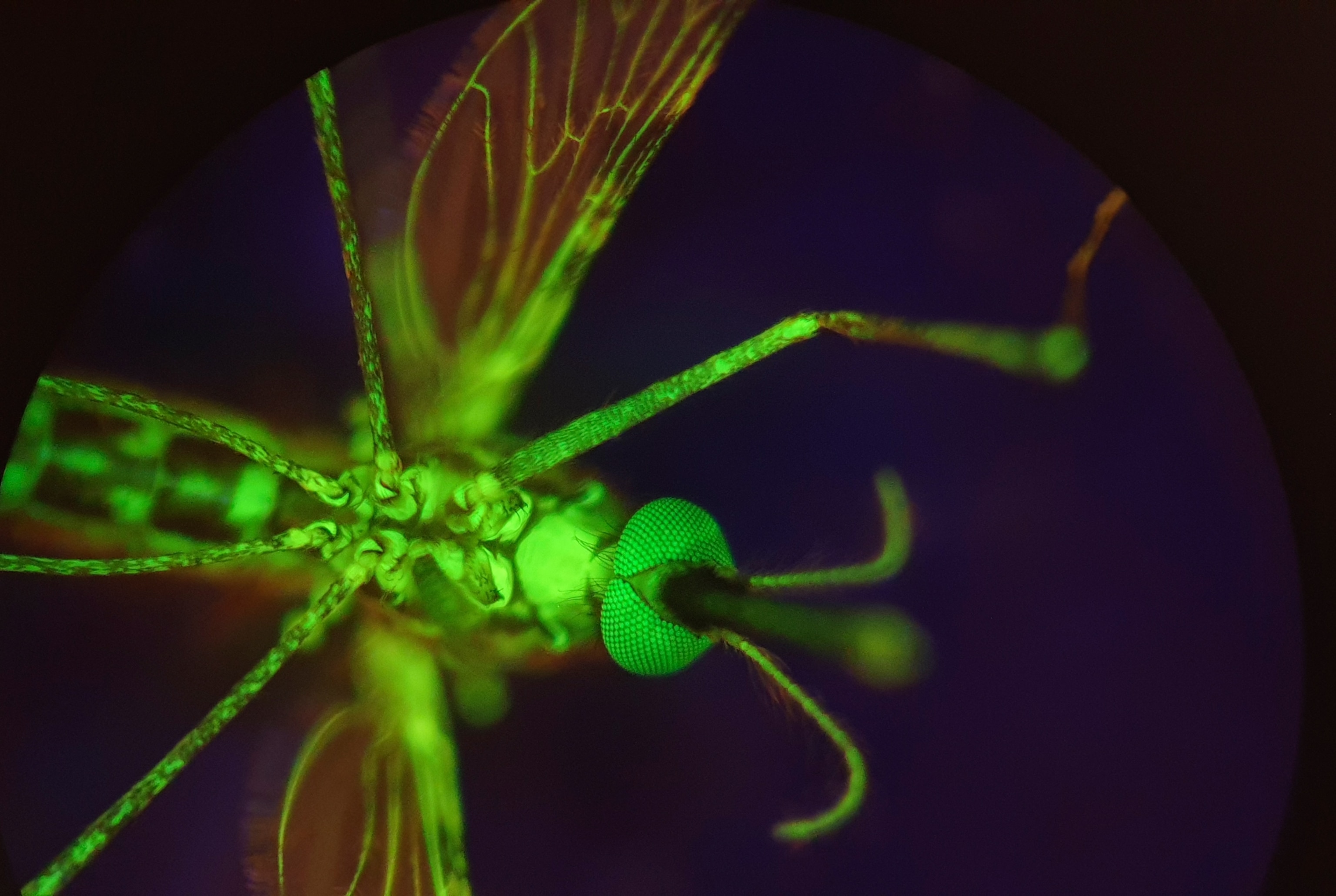
Malaria causes more than 600,000 deaths each year, and is just one of numerous deadly human diseases transported by mosquitoes. But what if we could make our blood poisonous to the parasites that crave it?
While it sounds like science fiction, the idea isn’t as far-fetched as it might sound.
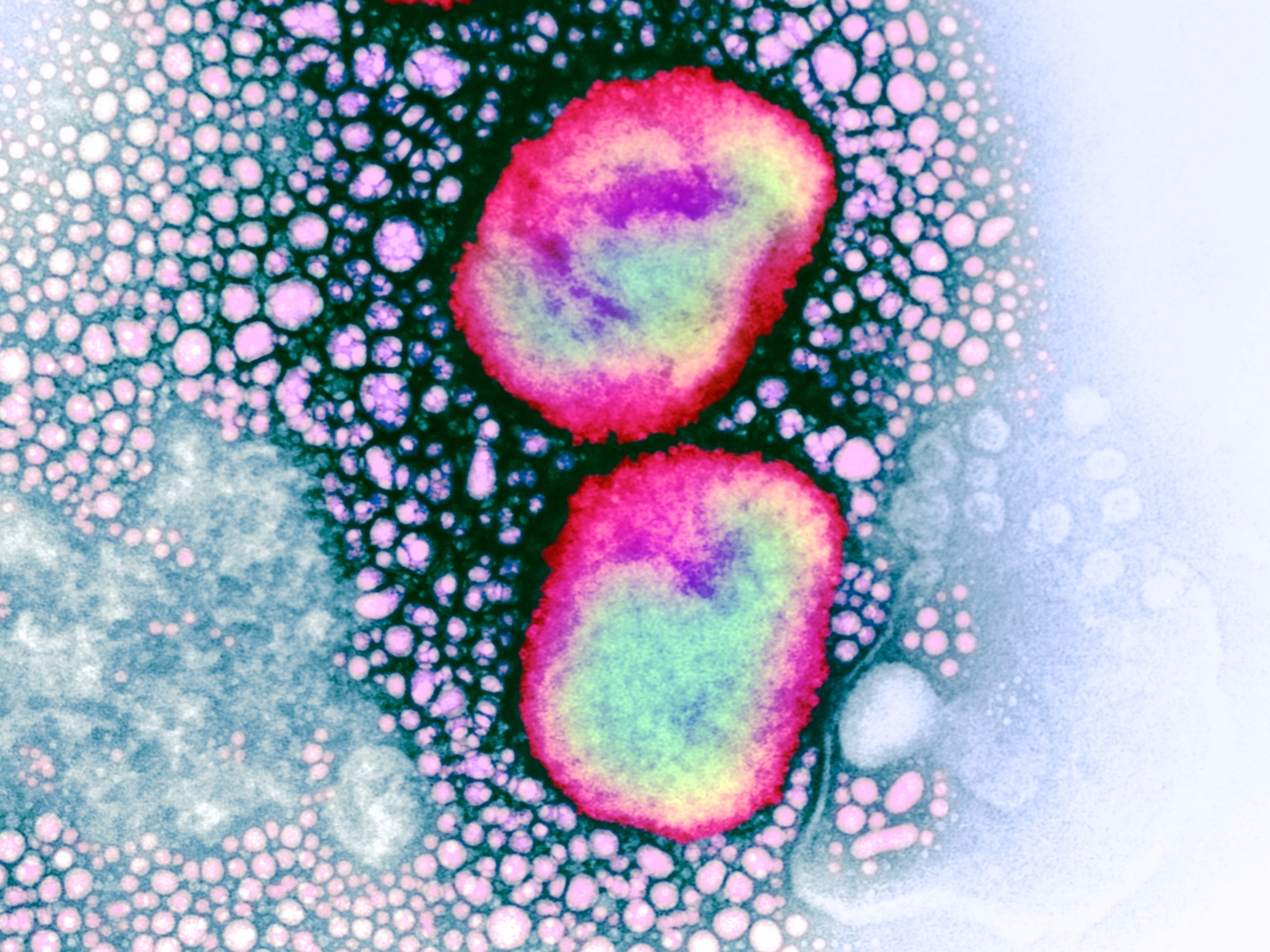
In a study published today in the journal Science Translational Medicine, scientists report that a drug known as nitisinone can turn human blood so toxic to mosquitoes that they die within a few hours of feeding on samples from patients who received even relatively low doses. What’s more, the drug remains effective for up to 16 days after the initial dosing.
It’s important to note that nitisinone does not itself protect against malaria infection. However, by killing the mosquitoes before they can lay eggs, the drug might be able to knock down disease-transmitting mosquito populations to the point that it breaks the chain of infection.
Like a vaccine that relies on herd immunity then, the promise isn’t in being individually immune to malaria, but rather working together as a community to snuff out an outbreak.
(What would the world look like without mosquitoes?)
While the researchers caution that such a tool is not intended to fully eradicate mosquito-borne diseases, it may prove helpful in conjunction with other strategies, such as insecticide-laced bed nets, malaria prevention drugs, and vaccines themselves. The new tool might prove especially effective in areas where mosquitoes have already developed resistance to other treatments.
“The interesting thing about this is that we’re using a drug that is already FDA-approved, because it’s used to treat rare genetic diseases,” says Álvaro Acosta Serrano, a parasitologist, vector biologist and coauthor of the study.
A drug with an interesting history
Inspired by a toxin in the Australian bottlebrush plant, nitisinone was originally intended for use as an herbicide. It worked by targeting an essential amino acid known as tyrosine.
A family of rare genetic disorders, such as tyrosinemia type I and alkaptonuria, occur when the body can’t properly metabolize that same amino acid. Researchers found that nitisinone could be an effective treatment, so the U.S. Food and Drug Administration approved it for use in humans in 1992.
“This is the only thing that has kept children with tyrosinemia type I alive,” says Acosta Serrano. “It's not a perfect solution, but it's the only thing.” While nitisinone causes an array of side effects in patients with such disorders, he says these populations typically have to take much higher quantities of the drug than would be needed for effective mosquito control.
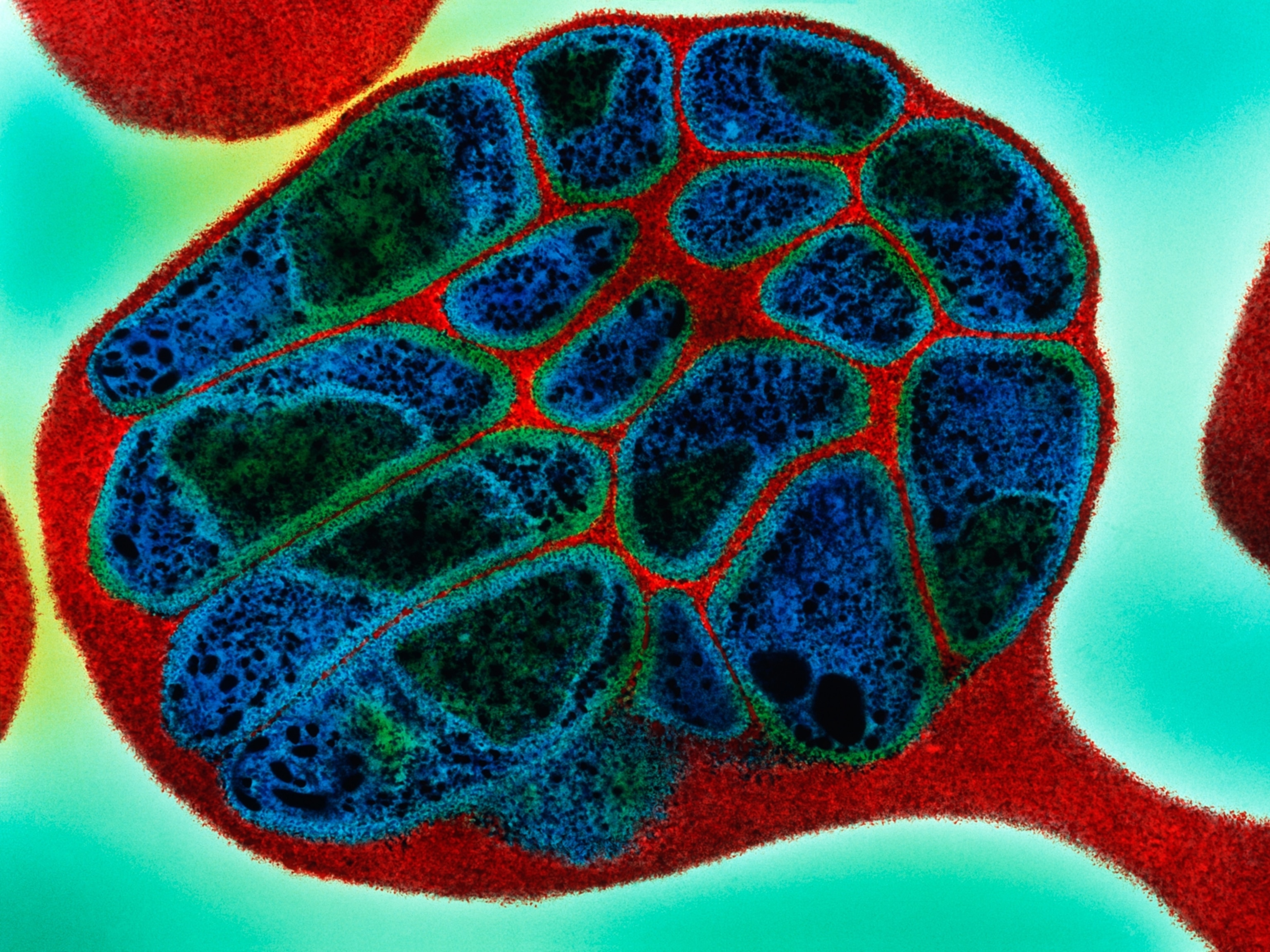
Interestingly, in 2016 a pair of researchers in Brazil named Marcos Sterkel and Pedro Oliveira discovered that blood-feeding insects, such as fleas, flies, and mosquitoes have evolved the ability to rapidly process tyrosine, which their bodies are flooded with after a blood-meal.
More importantly, they also learned that if you can disrupt that process, the insect will die.
Knowing that Acosta Serrano’s lab at the Liverpool School of Tropical Medicine in the United Kingdom worked on another disease-transmitting, blood-sucking parasite known as the tsetse fly, the researchers contacted him to see if nitisinone might have a role to play. Shortly after, the team expanded their work to look at nitisinone’s effect on mosquitoes.
And that’s how nitisinone went from killing plants to saving kids to potentially fighting against a deadly disease.
(Are we entering a new era of mosquito control?)
No silver bullets for malaria
Because nitisinone has already passed rigorous safety standards, repurposing the drug to combat mosquito-borne diseases would also require fewer approvals, says Acosta Serrano, who is now at the University of Notre Dame. For instance, nitisinone is currently cleared for use in newborns and young children, and no harmful events have been recorded in pregnant people. That’s one reason the results are promising.
“I think the study is very interesting,” says George Dimopoulos, a molecular biologist specializing in mosquito-borne diseases at the Johns Hopkins Bloomberg School of Public Health.
For starters, the idea that nitisinone might be useful in combatting mosquito-borne diseases is entirely new, he says. It’s also intriguing that side effects seem to be less than those seen in ivermectin, a drug which can also be used to prevent malaria transmission, and the efficacy greater.
Of course, Dimopoulos also pointed to several drawbacks.
“Malaria is a disease of poverty,” says Dimopoulos. “Anything that becomes expensive or costly is not going to work, especially for an intervention method like this, where you don't actually protect the individual from malaria, but you protect the population.”
The rarity of the diseases that nitisinone treats means the drug is still too expensive for widespread deployment. With more research interest, though, Acosta Serrano hopes that the costs of nitisinone could be reduced by as much as 80 percent.
The indirect nature of prevention could also be a roadblock. “It’s always tricky to convince people to take a drug that doesn’t protect them,” says Dimopoulos.
However, it may be possible in the future to combine a nitisinone treatment with an anti-malarial medication, he says. Likewise, the treatment might be made more effective by applying it to nearby livestock, which in effect work kind of like mosquito bait.
Similarly, because mosquitoes also rely upon nectar as a food source, scientists have also experimented with creating bags of nectar laced with insecticide that could target mosquitoes without exposing other pollinators to the poison.
“So in theory, you could also use this drug to expose mosquitoes through that technology,” says Dimopoulos. “You would not necessarily have to administer it to humans.”
Resistance is also a worry with any mosquito control method. But only time will tell if the critters could evolve to tolerate the toxin.
Whatever role nitisinone might play in the future, both Acosta Serrano and Dimopoulos agree that it will be most effective as part of a multi-faceted approach that is tailored to each population.
“In some places, drugs combined with the vaccines could work better. In other places, insecticide spraying and new technologies, like genetically engineered mosquitoes, for example, could have greater efficacy,” says Dimopoulos. “It’s a little bit like personalized medicine.”
“There is no silver bullet for malaria,” he says. “And I don’t think there will ever be a silver bullet.”