It’s possible to reverse diabetes—and even faster than you think
More than 830 million people worldwide have diabetes—a chronic, debilitating disease. But experts say it’s possible to recover with a few proven lifestyle changes.

Diabetes is a debilitating, life-threatening chronic illness that puts people at greater risk of blindness, kidney failure, and heart disease. But we’re also increasingly learning that it’s not a condition a person needs to live with forever.
One in 10 people in the United States and more than 830 million people worldwide have the disease—91 percent of them with type 2 diabetes; which, unlike type 1 diabetes, tends to develop in adulthood. About a third of Americans also have prediabetes—though more than 80 percent of them don't know they have it.
"Type 2 diabetes is like having termites in your home in that it doesn't show many symptoms at first, but can cause significant internal damage over time," says Osama Hamdy, senior staff physician at the Joslin Diabetes Center in Massachusetts. "The good news is, we have learned that if we catch the disease and intervene early, we can reverse it or induce remission."
Here's what it takes to reverse type 2 diabetes—and why remission can often happen faster than people realize.
What goes wrong in the body to cause type 2 diabetes?
Type 2 diabetes is caused by problems with insulin resistance or production.
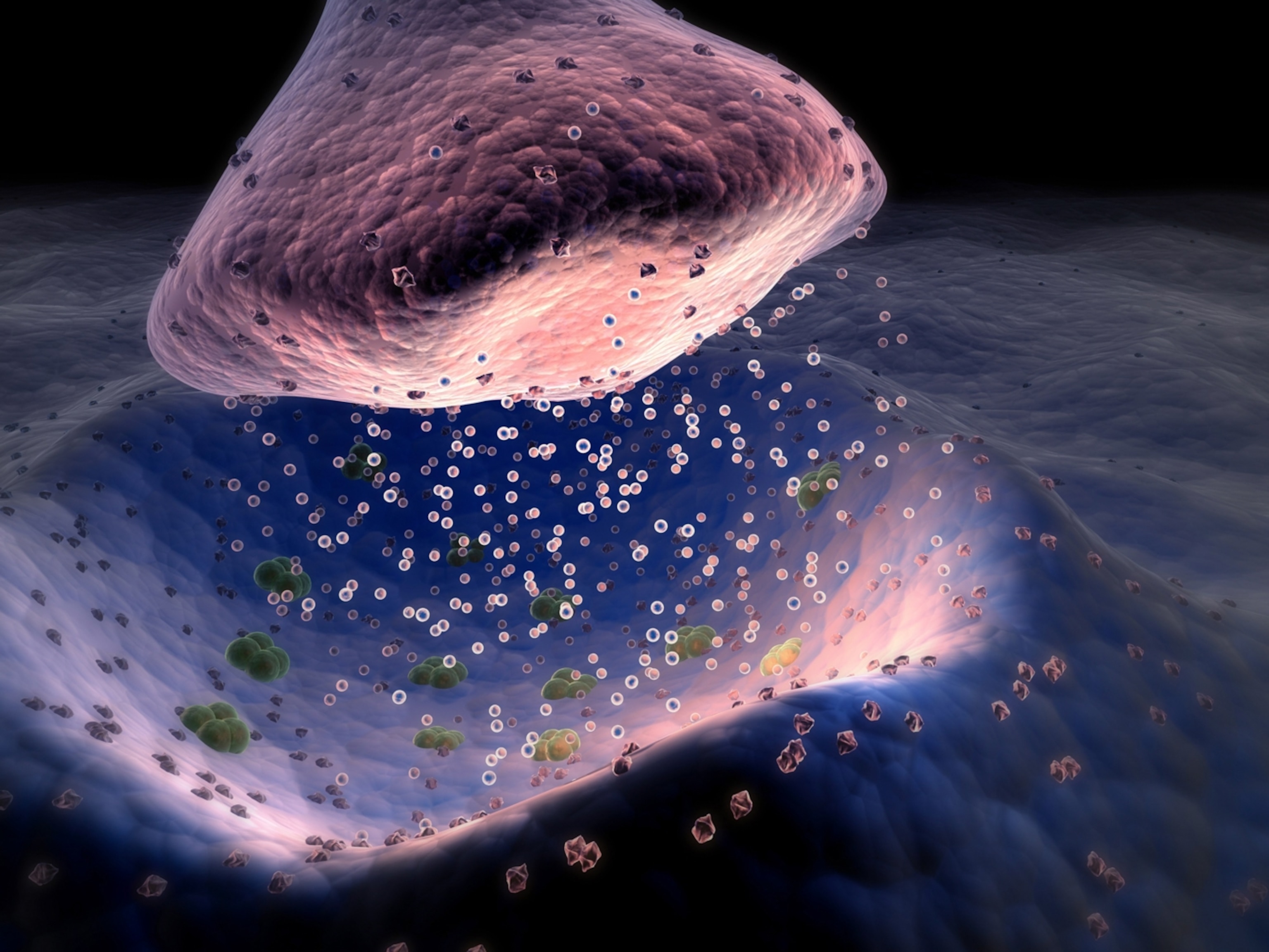
Insulin is a hormone released by the pancreas when the food we eat gets broken down into blood sugar, called glucose. It’s triggered to help move the glucose out of the bloodstream and into the body's cells, in order to provide our body with energy and our organs with vital nutrients.
"When someone has type 2 diabetes, this process isn't working properly," explains Sydney Blount, an assistant professor of medicine in the diabetes, endocrinology, and metabolism division at the University of Nebraska Medical Center.
(Why hibernating bears could hold a clue to treating diabetes.)
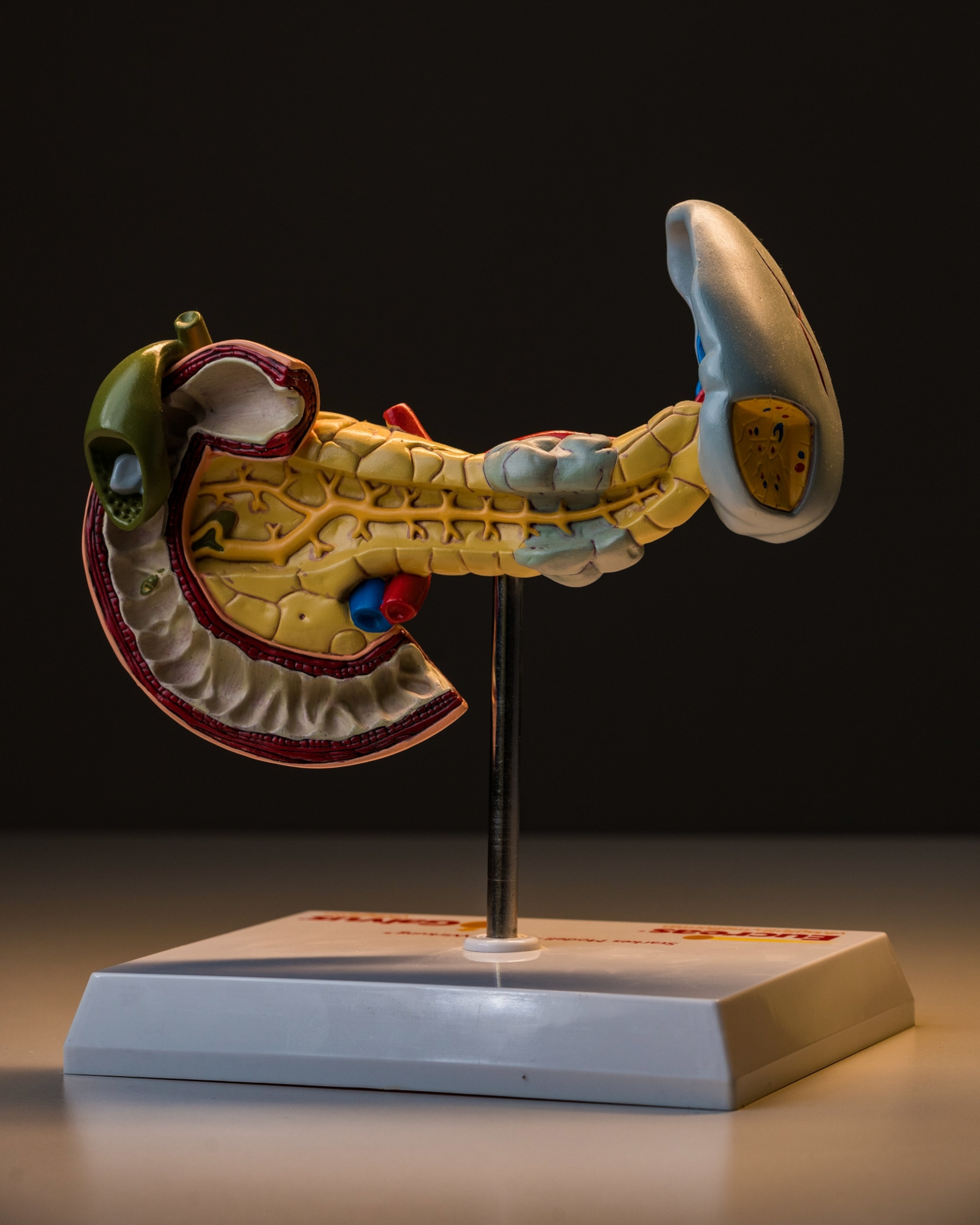
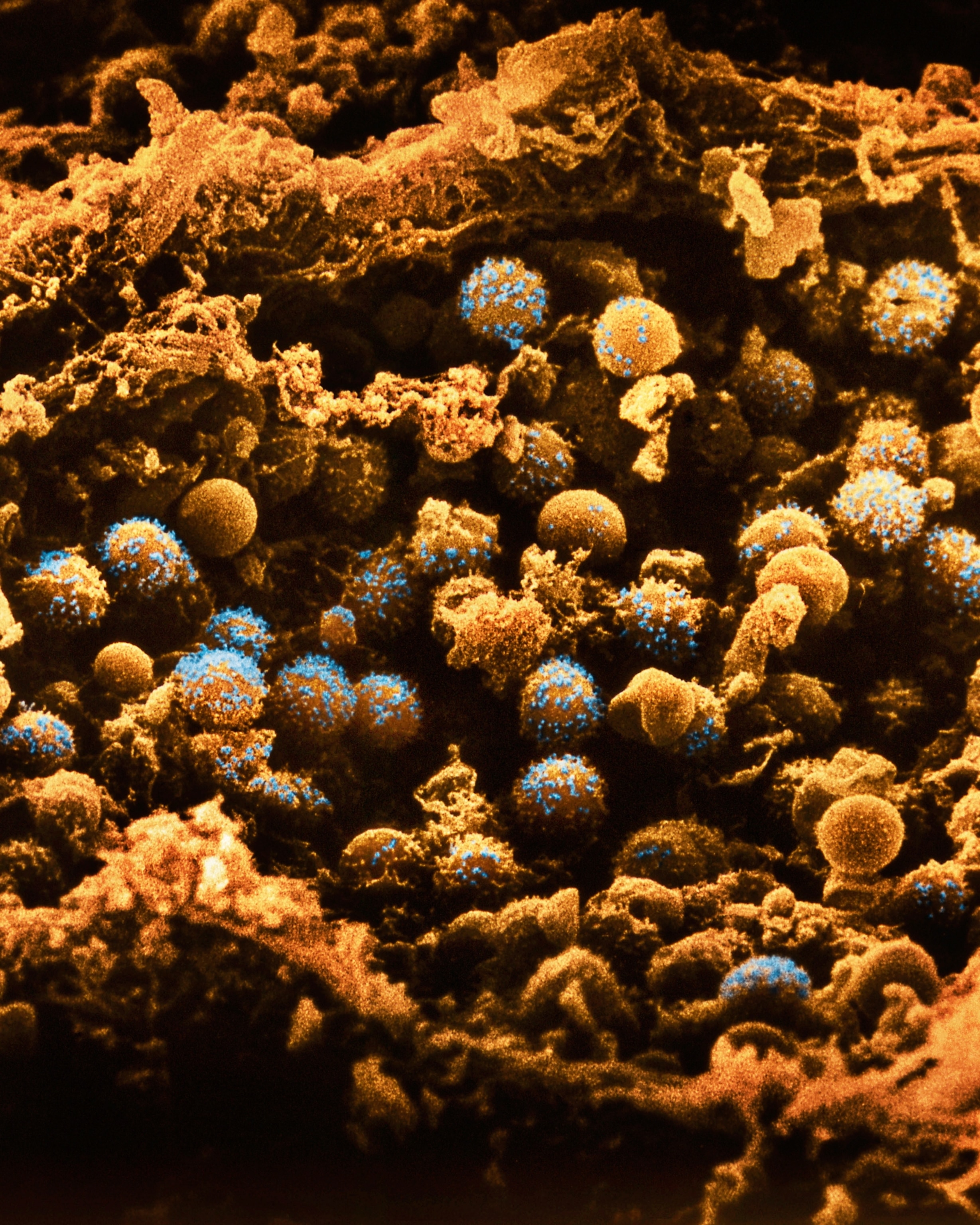
When insulin resistance occurs in cells—or when the pancreas can't produce enough of the hormone—the excess glucose in the bloodstream becomes toxic to organs and damages blood vessels throughout the body.
"Damaged blood vessels are why diabetes is the leading cause of amputations, erectile dysfunction, dialysis, dementia, blindness, heart attack, and stroke," says Elizabeth Vaughan, an associate professor at The University of Texas Medical Branch, who has co-authored diabetes research. Diabetes can also cause end-stage kidney disease, nerve damage, and several types of cancer.
The good news, though, is that "type 2 diabetes is driven by largely reversible metabolic abnormalities," says Dariush Mozaffarian, a cardiologist and director of the Food is Medicine Institute at the Friedman School of Nutrition Science and Policy at Tufts University. This means modest weight reduction, reduced stress, a healthier diet, and more physical activity “can all work to restore normal function of the body’s organs and tissues,” he says.
How weight loss can reverse diabetes
Weight loss is the most effective way to induce diabetes remission because "insulin resistance is closely linked to high levels of visceral fat," says O. Kenrik Duru, a professor of medicine at the David Geffen School of Medicine at UCLA who has authored multiple studies about diabetes.
Visceral fat is the internal fat surrounding organs such as the liver and the intestines, which is why people with a lot of visceral fat "tend to have larger bellies." Although we don't understand exactly how it occurs, Duru says, "we know that visceral fat communicates with the organs that absorb glucose from the blood, causing these organs to develop the insulin resistance that leads to type 2 diabetes."
(We’ve been measuring BMI since the 70s—but is the flawed metric still helpful?)
This is further evident as longitudinal research shows that a high body mass index (BMI) significantly increases one's risk for type 2 diabetes. "Even a 7 percent weight loss improves insulin sensitivity by 57 percent," says Hamdy.
The U.S. National Heart, Lung, and Blood Institute has an online tool that allows you to check your BMI, so you can know what “normal weight” category you need to aim for to be in the clear for developing type 2 diabetes—though the experts emphasize that BMI is not always the best measure of overall health.
How exercise helps reverse diabetes
Exercise makes a big difference as well as "physical activity promotes weight loss and also makes your muscles stronger and more able to absorb glucose from the blood," says Duru.
Exercise also "boosts insulin sensitivity" by increasing the ability of muscle cells to transport glucose from the bloodstream, says Vaughan "This is why I always recommend going for a walk after a meal."
(Walking is great for your health. Walking backward? Even better.)
To make sure you're getting enough exercise, the American Diabetes Association recommends getting a minimum of 2.5 hours of moderate physical activity a week or half that of vigorous physical activity—plus strength training at least twice a week.
How diet and lifestyle help reverse diabetes
Changing your diet can also improve your glucose levels "by minimizing blood sugar spikes and slowing digestion," says Vaughan.
Dietary changes might include reducing your total number of calories and limiting your intake of refined grains such as white bread, white rice, and white pasta as these foods can create glucose spikes in the body.
"It's also important to omit added-sugars intake entirely since they are empty calories and have a high glycemic index," adds Hamdy. Other foods high on the glycemic index you might want to limit include tortillas, crackers, noodles, certain breakfast cereals, and starchy vegetables like corn and potatoes.
(Giving up sugar can change your body for the better—within days.)
It's also important to increase the amount of fiber and protein you eat as fiber slows glucose absorption and improves satiety and protein helps build lean muscle mass. "Opt for minimally processed foods and lean meats," advises Vaughan, "and be sure to drink eight glasses of water daily as water helps your kidneys filter out excess sugar."
Along with weight loss and dietary changes, lifestyle improvements are also important. “Not getting enough sleep and experiencing too much stress both raise blood sugar levels,” says Vaughan. “Aim for 7 to 9 hours of sleep and practice relaxation techniques to reduce stress.”
An approach that tackles all these things “will lead to the best results,” says Sun Kim, an endocrinologist at Stanford University, who specializes in treating diabetes.
How long does it take to reverse type 2 diabetes?
Such a multifaced approach is so well proven that Hamdy says the Joslin Diabetes Center has created a program specifically tailored for diabetes remission. “80 percent of the patients admitted in the program are in diabetes remission within two years,” he notes.
But reversing the disease doesn’t have to take that long for everyone. "The shorter the diabetes duration and the higher the percentage of weight loss, the better the results," says Hamdy.
In fact, once you have lost the excess weight that first put you at risk for developing type 2 diabetes, he says, you may see remission-level glucose numbers in as little as days or weeks—the same way patients who have undergone bariatric surgery often do.
This can also occur through significant dietary improvements if that’s what was causing glucose levels to spike. "A person recently diagnosed with type 2 diabetes can rapidly get blood sugar to normal through diet changes," says Kim, "especially if someone suddenly cuts out a 'big-ticket item' like six regular sodas per day."
Getting back to healthy glucose levels is only the beginning though. Diabetes isn’t considered to be in remission until “glucose numbers are below the threshold for diabetes diagnosis for at least three months without diabetes medications,” says Kim.
In other words, you have to get to remission-level glucose numbers and stay there. And the disease can always return with significant weight increases or the return of bad eating habits.
"It's important to remember that type 2 diabetes is preventable," offers Blount, "and prevention is the best medicine."